Treatment costs for chronic kidney disease (CKD) and end-stage renal disease (ESRD) are high and rising dramatically, putting self-funded health plans at risk. Meanwhile, most health plan members with moderate kidney damage are unaware they have it until it has progressed to the point of requiring difficult, expensive treatment. To learn more about the steps health plans can take to control costs and provide better, healthier options for their members, SmartBrief spoke with Renalogic CEO Lisa Moody.
Why is chronic kidney disease leading to dialysis called “the silent epidemic,” and why should companies care about controlling CKD treatment costs?
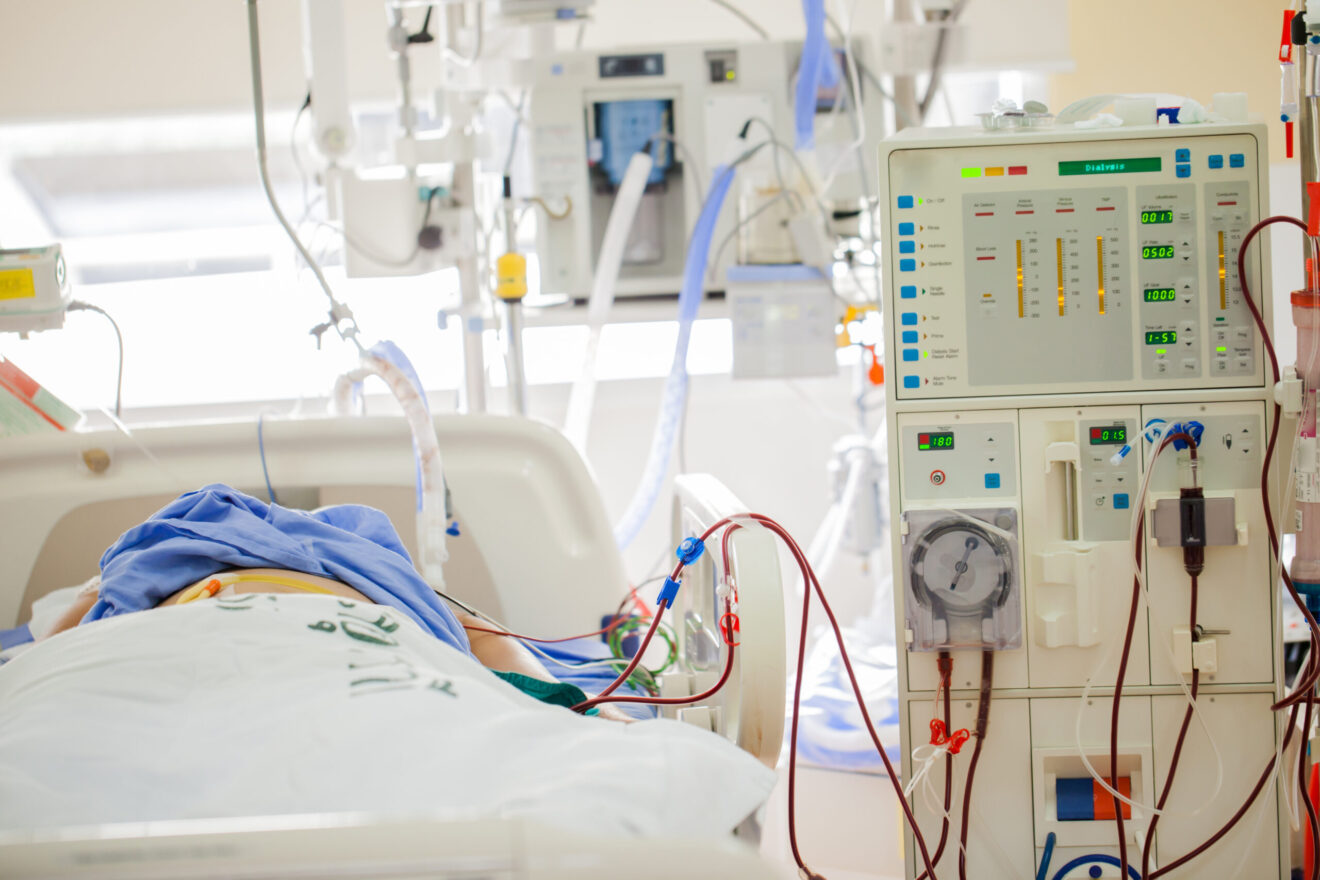
It has become clear that even with a high focus on employee wellness, health in America is declining. As the risk factors and the comorbidities of a sedentary lifestyle and the typical American diet continue to accrue, more and more people are at risk for CKD and don’t know it. CKD is called the silent epidemic because it exhibits no symptoms until the very late stages, leaving many individuals unaware they have it until it has progressed to a dangerous reduction in kidney function. Late-stage CKD can become very expensive to treat and, if allowed to progress too far, will result in kidney failure requiring dialysis.
The Renalogic Kidney Dialysis Prevention Program was launched to help our clients identify both CKD-diagnosed members and those who are undiagnosed but highly likely to have CKD, and intervene with their members to prevent their progression to end-stage renal disease.
What is the difference between cost savings and cost avoidance for dialysis, and how is Renalogic doing both?
Cost savings are achieved with Renalogic’s Kidney Dialysis Cost Containment program, which reprices the cost of claims using a usual and reasonable method for determining the reduced cost. Our clients see an 85% to 91% reduction off total billed charges.
Cost avoidance is achieved with Renalogic’s Kidney Dialysis Prevention Program, which identifies and proactively engages members at risk for the progression of CKD. We are proud to say we have never had an individual progress to dialysis while they were engaged in our Kidney Dialysis Prevention Program. This avoids potentially catastrophic future costs related to dialysis and the treatment of kidney disease and also helps the individual achieve a healthier, higher quality of life.
What makes your CARE plan for the Renalogic Dialysis Prevention Program successful?
Renalogic is the only cost-containment company with on-staff registered nurses certified in renal care and case management, and they actively help members avoid progression to dialysis. The success of our program is based on the relationship of trust that is built between the nurse and the participating member, leading to the incorporation of healthy behaviors into a member’s daily routine.
Having an advocate in a member’s corner is key to understanding the variables associated with kidney disease and dialysis, as well as the options for treatment eligibility under Medicare. Ultimately, Renalogic specialists are advocates for plan members and can help health plans and members navigate the system successfully.
What is the impact on members currently on dialysis when a company uses Renalogic?
For members already dialyzing, our nurses educate them on home modality options, Medicare coverage, nutrition and fluid intake, lab numbers, transplant options and how to maintain a healthy lifestyle while on dialysis.
Does Renalogic use reference-based pricing or a derivative of Medicare for pricing of dialysis claims?
Renalogic does not use reference-based pricing or a derivative of Medicare. While RBP can be a good strategy for self-funded health plans, it is imperative that dialysis be excluded and managed differently. There are legal risks to using a RBP or a derivative of Medicare pricing strategy with kidney dialysis because it is a complex procedure that is handled differently by Medicare than any other treatment. There are up to 18 variables built into how Medicare prices a claim, and it is impossible to determine what Medicare would pay. Using a simple percentage of Medicare exposes a plan to risk of lawsuits, and there have been several recent cases against simple Medicare repricing of dialysis claims.
Instead, Renalogic uses both public and private geographical and economic data to determine a usual and reasonable price for kidney dialysis services.
On average, the cost per month for dialysis is $100,000 — or $1.2 million annually. We deliver a more than 85% reduction of the total billed amounts, which is a difference of $45,000 per month or $540,000 annually. We also have the most defensible administrative record and have never lost a provider appeal.
Renalogic acts as an advocate for self-funded health plans and their members to help control the costs of kidney disease treatment and stop its progression. Learn more at www.Renalogic.com.