Traditional measures of heart disease are falling short, and there are untapped opportunities to diagnose heart disease faster and provide more complete information to the care team. SmartBrief recently spoke with Joseph Jasser, chief of value-based care for Cleerly, to find out how a new solution can flag heart disease sooner while informing personalized treatment plans that can help avoid unnecessary, high-cost procedures and improve patient care.

What are some shortfalls of traditional measures of heart disease and conventional testing?
The markers we have traditionally used tend to be surrogate markers of other disease processes. For example, low-density lipoprotein (LDL) levels in the blood is a long-standing test used as an indirect indicator (surrogate) of high cardiovascular disease (CAD) risk. We look at LDL and HDL to detect the level of fats (lipids) within our blood, and those are markers of just fat (lipids) and not necessarily of the actual disease process — atherosclerosis.
We’ve also been managing signs and symptoms by bringing people in for stress tests. In the US, the most common tests performed to diagnose CAD are functional stress tests and coronary angiograms. However, nearly 90% of stress tests are normal. In addition, functional stress tests have low specificity with frequent false positive findings of roughly 55% and a false negative rate of roughly 30%. That leads to two significant issues: patients are discharged with undetected CAD due to a false negative, or are referred for unnecessary invasive procedures.
We’ve been looking at markers that don’t identify the disease, and we’ve been managing the disease process with tests that have a high rate of false positives and false negatives. As clinicians, historically we haven’t been managing the atherosclerotic condition that is causing the heart attacks or more importantly, the disease process itself.
What are the differences between those methods and coronary CTA with artificial intelligence quantitative CT?
With a nuclear stress test, we monitor blood flow through the coronary vessels and identify areas with ischemia, or decreased blood flow in the heart musculature. However, as I noted earlier, there is a high rate of false positives in nuclear stress testing due to many variables, such as atypical dynamics of flow within the heart muscle, the image quality and noise and finally, the differences and consistency with which physicians interpret the images.
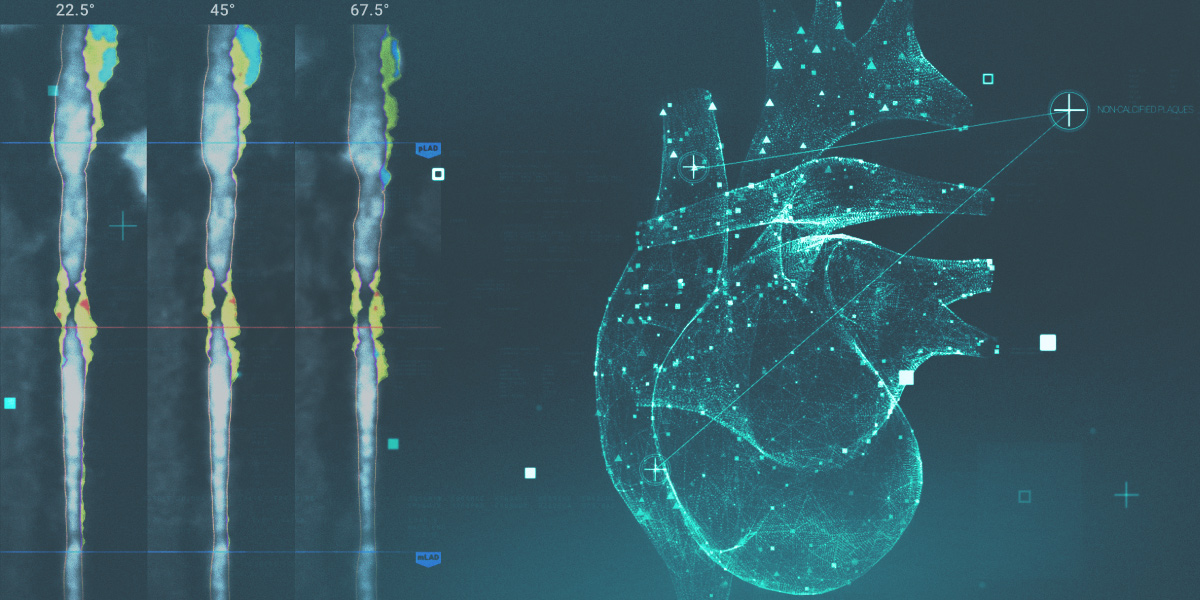
With a standard CCTA, we scan the heart on the off beats and look at the coronary vasculature. These images allow us to determine the flow and stenosis, as well as the disease within the blood vessels that causes stenosis.
Adding atherosclerosis imaging quantitative computed tomography (AI QCT) involves breaking down the pixels of the CT image into subpixels and determining the levels of gray within those subpixels. This provides more detailed data that can be used to determine the density, formation and type of plaque lining the blood vessels. This, in turn, allows us to identify and quantify the type and density of plaque. And it’s the type of plaque that has been found to be correlated with heart attack. This information provides clinicians insight into how acute and/or how calcified or chronic that plaque is. All this is completely new for the medical community, and our ability to measure and quantify plaque allows for earlier interventions with avoidance of unnecessary and high-cost procedures.
What populations could be identified earlier, and how could this improve patient care and help avoid unnecessary, high-cost tests?
The ideal situation would be identifying patients at risk for acute myocardial infarction earlier in the process. These are typically patients between the ages of 50 and 65 with signs and symptoms and/or significant risk factors. By scanning those individuals, as I noted earlier, we are able to measure the type of plaque and identify the overall disease burden, and tailor their treatment to the findings from the CCTA with AI QCT.
Another goal is to supplement or replace the nuclear stress test process for patients who are not in crisis but present at the physician’s office with atypical chest pain or stable chest pain. In these cases, rather than doing a nuclear stress test, a CCTA with AI QCT could identify the type of plaque and the plaque burden, as well as the stenosis, and could provide clinicians with more definitive information. This would allow the physician to personalize their medications and treatments, and avoid unnecessary procedures downstream for patients.
How can CCTA with AI QCT help providers with care management?
Based on the clinical findings within the CCTA with AI QCT, the identification of the type and density of plaque helps physicians determine which medications would be most effective for conservative treatment. Also, given the superiority of CCTA with AI QCT over nuclear stress tests for identification of CAD, the physician can more definitively assess whether they need to perform a coronary catheterization in addition to conservative treatment. This approach would allow more personalized patient management as well as avoid unnecessary procedures.
As an example, historically, we used to look at calcium scores to determine whether the plaque within blood vessels has a high density of calcium and extrapolate that to how much disease is present. What we discovered is that those are stable plaques that don’t necessarily need aggressive treatment. Plaques that are high-fatty plaques are unstable and need aggressive medical treatment. By identifying the makeup of the atherosclerotic plaque on the CCTA with AI QCT, we can determine the best intervention and/or the most appropriate medications needed to treat the disease.
What impact is this expected to have on value-based care initiatives?
If we can identify the patients who would benefit most from CCTA with AI QCT, we can move treatment upstream to the primary care provider. By providing clinical insights that help providers identify the disease, create a more personalized treatment plan and aggressively treat the disease earlier, we can avoid downstream expenses such as hospitalizations and unnecessary procedures such as coronary catheterizations. By treating the atherosclerosis conservatively through aggressive medication management, we can also help decrease the incidence of heart attack by roughly 40%, which also lowers the incidence of congestive heart failure due to heart attack.
These are significant cost drivers for value-based care providers. By leveraging CCTA with AI QCT, primary care physicians will have the opportunity to manage patients conservatively and avoid or altogether eliminate the referral to cardiology.
Dr. Joseph Jasser is chief of value-based care for Cleerly. Prior to joining Cleerly, he was chief medical officer of Vesta Healthcare and previously, he was the principal owner/chief medical officer of bclinical, PLLC, where he provided clinical consultative services for clinical delivery organizations and medical groups. Dr. Jasser earned his bachelor of science degree from The Ohio State University, his medical degree from The Ohio State University College of Medicine and an executive Master of Business Administration from Washington State University.